The term "Trigger Points" was introduced by Janet Travell (1901-1997) in 1952, although the concept had been known in "official" medical circles for at least a century, although in a more vague manner.
But we believe we can say that the concept was well known in traditional medicine, though of course not in the scientific details accurately described and systematized by Janet Travell, an exceptional scholar who among other things was also the personal physician of J. F. Kennedy, and the official physician of the White House during the Kennedy and Johnson administrations.
J. Travell dedicate her entire career to the study of Trigger Points, which from now on will simply be written TP.
Initially a cardiopulmonary specialist, Janet Travell noticed that 1) the pain was the main complaint of his patients, and 2) the main cause of pain was myofascial in nature, and in particular muscular. This regardless of diagnosis of the patient's illness.
So it can be said that J. Travell began to focus on the essential predominance of the muscular system as a cause in the vast majority of pain syndromes in patients.
Her research is at the same time a critique of academic medicine, which has become increasingly technologized and specialized and yet has culpably ignored the muscular system to such an extent that there is not, among all medical specialties, the "muscle specialist"!
Now devoting full time to the study of myofascial syndromes, J. Travell, later assisted by Dr. David Simons, began to focus on the crucial concept of the muscle pain syndrome that she called '"Myofascial Trigger Point" (Travell J, Rinzler SH: The myofascial Genesis of Pain. postgrad Med 11:425-434, 1952).
Travell's discovery was therefore that of identifying and describing the Trigger Points (TPs) as muscle entities specific having
characteristics. More generally, there are also extra muscular Trigger Points, fascial TPs in particular that cause similar pain syndromes. However, these other varieties of TPs seem less easily categorized and at present their understanding is not so advanced as in the case of the muscular TPs.
A partial synthetic definition of TPs made by Travell is: a local area in an extremely irritable and painful nodule in a taut band of muscle tissue.
Since we are working from a practical and empirical perspective, it is recommended to learn such a definition by memory although incomplete, because it will allow us to reach a formula that will make it possible to identify, and then treat, the TPs, even without necessarily having to memorize the several hundred muscles in the human body (650-850 depending on the classification) and the thousands of possible TPs. It is therefore desirable to formulate synthetic criterion for the detection and treatment of TPs on the basis of a few basic concepts and simple manual inspection.
Let us pause for a moment, then, on the above partial definition. It alludes to a nodule, a tight bundle of fibers, and a localized, painful knot. So for the purpose of manual inspection of a muscle, one will seek a bundle of muscle cells that are in an abnormal state of tension, which will give us often the impression of a tight rope.
Along this "rope", we will try then to locate small nodules of consistency even more rigid than the tense bundle (if it weren't so it would not be possible to differentiate them from the muscle fiber bundle n wich the nodule is embedded). At this point, once we find the lump, the TP is almost found, except that it occupies an even smaler area located within the nodule itself.
Clearly then, following this method one can find any muscle TP without necessarily having to memorize the names and shapes of the eight hundred and more muscles of the human body. All is really needed is to develop an adequate touch sensitivity .
The definition given above though, is for all practical purposes to be considered partial and should also be augmented by introducing the concepts of pain and recognized pain .
When applying pressure to the TP, pain is caused that the subject recognizes as familiar and already experienced either in present form or in an event of the past. Moreover, in many cases the pain in question emerges at a certain distance from the TP involved. In fact a feature of many (but not all) TPs is to cause pain in localized areas at some distance from the TP itself.
Because some TPs do not obey the rule of referred pain, then referred pain can not be a necessary condition for muscle lump to be a TP, but the preponderance of referred pain in TP syndromes suggests that if a nodule causes muscle pain reported elsewhere as a result of pressure, then one should believe to be in the presence of a real PT.
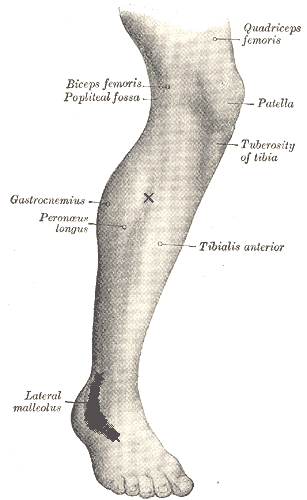
For example, if when compressing the proximal Peroneus just below the knee, one causes pain in the area of the lateral Malleolus, then one can say without doubt that one si dealing with a TP. ( See the image where x is the TP and the gray area around the ankle is referred pain). The case in question is typical of ankle sprains, where pain continues long after the trauma, the residual pain being perpetuated by the peroneal TP.
At any rate, a complete definition of TP must include the notion of evoked familar pain, but not of referred pain, because in not al cases does the pain appear at a distance from the TP.
So in summary,
Definition of Trigger Point (TP): localized area located in an extremely irritable and painful nodule in a taut bundle of muscle tissue, and recognition by the patient of pain evoked by pressure of the PT as a pain known or familiar.
To complete the general description of the TPs, we must now understand what happens at the microscopic cell level , after which one will have all the elements necessary to proceed to the practical applications, that is to the treatment and care aimed at reducing the pain and dysfunction associated with TPs.
It is known that muscle cells are longitudinal, and contractions of these cells occurs through units called sarcomeres, which contract and release by acting as microscopic pumps and circulating oxygenated blood and nutrients into muscle tissue. As a result of excessively prolonged contraction, this pump effect stops and creates a local energy crisis of lack of oxygen and accumulation of metabolic waste. The sarcomere becomes unable to release the contraction and assumes a state of mechanical and permanent rigidity.
The sum of several sarcomeres in this state originates the abnormal nodule of the TP, which in turn gives rise to the bundle of fibers that runs along the entire muscle. As a result of this condition then the whole muscle is found in a state of hypertension and in particular the fascia and the muscle-tendon and tendon-bone interface is to suffer chronically. Therefore, a PT located in the center of a muscle can give rise to pain in the extremity of the muscle and at the tendon attachment (see the example shown above peroneal).
It is also obvious, that since the sarcomeres involved are stuck and unable to relax spontaneously, it becomes necessary to intervene to stop the mechanical contraction and paroxysmal local energy crisis. From this observation, Janet Travell's ideal clinical treatment was to pierce the TP with a needle, preferably at the same time injecting a local anesthetic solution. However, we believe that there is no need for gory interventions and a specific massage performed by a person with appropriate technical expertise can cure without having to pierce the TP tissues, located in areas often delicate and full of nerves and blood vessels such as p. eg. the neck or the inside of the thigh. So a more sensible therapy, is that of the manual processing by means of fingers, knuckles, elbow, or at least using appropriate tools such as Theracane and Knobble,of which we will be talking later when we discuss the therapeutic practice of PT .
So we conclude this first brief introduction to TP where we established the theoretical foundations and the basis for the practical treatment of these small but vocal devils of our muscles.
